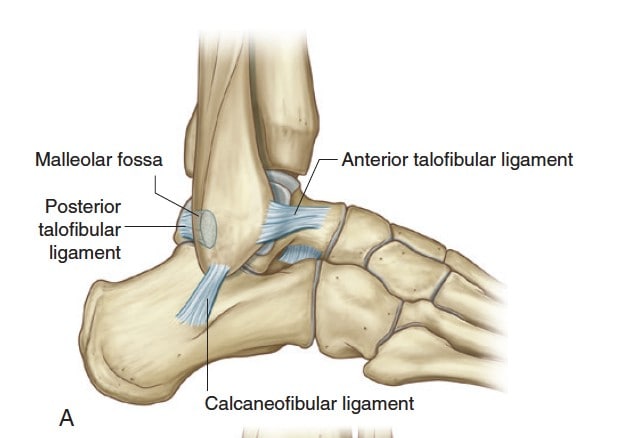
An ankle sprain occurs when ligaments in the ankle are stretched or torn. Ligaments in the ankle are bands of fibrous tissue which hold bones in proper position and stabilise the joints. There are three main groups of ligaments in the ankle, the medial (inner) ligament, and the lateral (outer) ligament complex, and the syndesmotic ligaments.
Most simple ankle sprains occur at the lateral ligament complex, which consists of 3 different ligaments. Of these, the anterior talofibular ligament is the most commonly injured. More severe injuries can result in tears of more than 1 ligament.
Signs and symptoms of an ankle sprain include:
If you are able to take a few steps while bearing weight on the injured ankle, it is a sprain and not a fracture!
Most often, an ankle sprain occurs when one has their foot planted firmly on the ground but suddenly makes a change of movement. This can happen during a fall when someone steps on your foot and often during sports when one has an awkward landing or pivots. This causes the ankle to roll inwards, and the ligaments may stretch or tear.
In some cases, when the foot rolls outwards and the ankle rolls inwards, this will result in the medial ligament being sprained.
Ankle sprains can affect you in different ways depending on the severity of the sprain, and which ligament was affected. Sprains can be graded based on severity, with grade 3 tears meaning that the entire ligament is torn. More severe tears tend to cause more discomfort and may take longer to heal. For the majority of patients, ankle sprains will heal without complications. A small percentage of patients, however, will develop symptoms due to chronic ankle instability. The more severe the initial tear, and the more ligaments affected, the more likely that this chronic instability will occur.
Patients with chronic ankle instability will find themselves having pain when walking on slopes and stairs and have difficulty with athletic pursuits. They might even feel that the ankle ‘gives way’ very easily, and might fall more frequently, leading to further injuries.
Based on your medical history, your doctor will perform a focused examination on your ankle. This will include checking the range of ankle movement and feeling the ankle joint and ligaments/tendons for pain. He/She may also test if the ankle is stable by pulling on it (anterior drawer test).
As part of the work-up, your doctor may order X-rays to check if there is a fracture, and may also recommend an MRI scan to evaluate the state of the ankle ligaments.
Most patients with ankle sprains can be managed without surgery. However non-surgical treatment carries the risk of chronic instability, especially in severe ligament tears, or tears involving more than one of the lateral ankle ligaments.
1. R.I.C.E. method
This method should be carried out immediately as first-aid when one realises they have injured their ankle. It includes:
2. Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can be taken to help reduce pain and swelling in mild sprains.
3. Usage of orthotics (medical devices to support movement)
4. Immobilisation
For more severe sprains, immobilisation of the ankle may be necessary to prevent sudden movements and provide support. This can come in the form of a removable plastic device known as a cast-boot, an air-filled or gel-filled ankle brace, or a short leg backslab (half cast) to be worn for a couple of weeks.
Physical therapy is very important for recovery from an ankle sprain as it can help ensure the ankle heals properly and does not lead to further complications. Rehabilitation exercise can begin soon after the injury, especially for less severe injuries. The main goal of physical therapy would be to restore range of motion, strength, flexibility, and stability. Proprioception (balance) training, endurance, and agility exercises are also a part of physical therapy. This type of exercise can help prevent future ankle sprains or instability.
Surgical treatment is an option for patients with chronic instability, and in patients who want to minimise the risk of chronic instability. Currently, surgery is conducted using arthroscopic techniques (keyhole surgery) and is safe with minimal down time.
During surgery, small holes are made in the front of the ankle. This is used to access the joint and to allow the passage of small instruments for the repair of the torn ligament. In most cases, only the anterior talofibular ligament needs to be repaired. This repair is conducted using sutures, and no metal implants are necessary.
After surgery, the patient is placed in a protective shoe, which protects the repaired ligament for up to 4 weeks. Sutures will be removed after 2 weeks, and most patients will be able to walk without crutches 2 weeks after surgery.
Evidence suggests that adopting a strategy of early repair, rather than a wait and see approach gives better early outcomes in terms of ankle function and patient’s ability to do sport. This suggests that all physically active patients might benefit from early repair, especially if they intend to return to sport.
Based on the severity of the ankle sprain, the period for recovery will vary. For mild ankle sprains, patients are usually able to make a full recovery within 7-15 days. In more severe cases, it may require a few months of physiotherapy before ankle function and strength are fully restored. If you play sports, returning to the sport should only be when the symptoms of the ankle sprain have been resolved.
Patients who have opted for surgery will usually be able to begin rehabilitation 4 weeks after surgery and can expect to return to sport 6 to 8 weeks after surgery.
For an assessment of your condition, please book an appointment with Dr. Yong Ren.