Joint cartilage is a connective tissue with a smooth and slippery surface, found in joints such as the knee. It allows bones of the knee joint to slide over each other smoothly, so as to minimise friction during movement.
Cartilage Lesions are common injuries that refer to holes that develop in cartilage. These holes may be the result of direct injury from accidents or falls.
Cartilage lesions may also develop in patients who have thinned out cartilage from regular wear and tear. In this case, the thinning of the cartilage makes it easier for the cartilage to be injured. Depending on the severity of the condition, the injury may range from a soft spot in the cartilage to cracks and fissures, to a hole that exposes the underlying bone.
As cartilage lacks blood supply, the body cannot repair and heal the cartilage lesions on its own. Eventually, as the lesions become more widespread and larger, the patient develops a condition known as osteoarthritis, which can lead to severe joint pain and limit a person’s ability to perform activities of basic living.
Some signs and symptoms include:
If any of these apply to you, you should seek medical attention as soon as possible.
Based on your symptoms, the doctor will conduct a focused examination on the injured limb, which would include an assessment of your ability to sit, stand, walk and lift your legs. The doctor will also feel around the knee for any spots that might be painful. This will give a clue as to the underlying cause of your knee pain.
The doctor will usually order Magnetic Resonance Imaging (MRI), a radiological test that uses radiofrequency waves in a strong magnetic field to generate two- and three-dimensional images of bones, muscles, tissue, tendons, nerves, ligaments, and blood vessels, to show problems that are linked to knee pain. It can also ensure that the knee pain is not due to a subchondral bone marrow lesion, a condition in which bone under a patch of damaged cartilage is also injured.
Cartilage lesions are irreversible. However, there are several surgical techniques that can help to regenerate cartilage. In general, most patients with cartilage lesions should undergo cartilage restoration to prevent downstream knee osteoarthritis.
Non-surgical options are considered adjunctive to surgical treatment and can be taken in conjunction with surgery. These methods do not heal the cartilage lesion but may provide some symptom relief.
Prescription medications and nonsteroidal anti-inflammatory drugs may be taken to relieve any discomfort as a result of cartilage lesions.
The use of an offloading brace is an option to provide stability, support, and pain relief to the affected knee. As its name suggests, an offloading brace effectively transfers the pressure from one side of the joint to another to reduce discomfort.
Most of the surgical options for cartilage lesions in the knee are performed using arthroscopic techniques (keyhole surgery). Arthroscopic techniques allow for faster recovery from surgery due to the small incisions used.
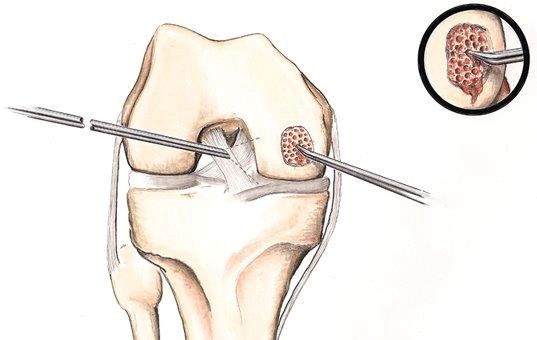
During this procedure, after gaining access to the knee using keyhole techniques, the hole in the cartilage is identified, and the cartilage is trimmed. Holes are then made in the bone underlying the cartilage lesion (microfracture). This is to allow bone marrow to enter the defect. Bone marrow contains stem cells, which have the potential to heal the hole by becoming cartilage. To aid the process, a collagen patch is placed over the cartilage lesion, which traps and concentrates the stem cells.
ACI is a double-step procedure that takes place across a few weeks. First, healthy cartilage-forming cells are taken from another area of the knee, and then cultivated and multiplied in the lab for several weeks. Second, the cultured cartilage cells are injected under a layer of bone-lining tissue stitched to the defect, to form new cartilage.
MACI is a double-step procedure that takes place across a few weeks. First, healthy cartilage-forming cells are taken from another area of the knee, and then cultivated and multiplied on a patch-like membrane in the lab for several weeks. Second, the cultured cartilage cells are implanted via the membrane glued to the defect, to form new cartilage.
In OATS, healthy cartilage tissue is taken from another area of the knee and grafted to the area of the damaged cartilage. The graft is taken as a cylindrical plug of cartilage and bone, matched to the surface area of the defect, and impacted into place. This leaves a smooth cartilage surface in the joint.
If the cartilage lesion is deemed too severe, your doctor may advise that you undergo knee replacement surgery rather than keyhole surgery.
In addition to the options discussed above for treatment of cartilage lesions, if you are found to have a bone marrow lesion (as detailed above), your doctor may also recommend that you undergo a procedure known as subchondroplasty. In this case, the damaged bone underlying the cartilage is drilled and an absorbable cement is injected to reinforce the bone.
Regardless of the method used, patients who have undergone surgery will have their sutures removed after 2 weeks. They may also be asked to wear a brace for up to 6 weeks as the cartilage recovers.
After treatment, patients are recommended to undergo proper individualised rehabilitation. The time taken for complete recovery could be up to three to six months, depending on the severity of the lesion and the type of procedure carried out. Physical therapy, such as flexibility and strength exercises for the muscles and tissues around the knee joint, should be carried out for rehabilitation and recovery, as recommended by the physical therapist. Even after the pain is gone, it is encouraged to continue to practise the techniques and exercises regularly.
For an assessment of your condition, please book an appointment with Dr. Yong Ren.