Foot arch pain, also known as arch strain or arch discomfort, refers to a sensation of pain or discomfort in the area of the arches of the feet. The arches of the feet are formed by the bones, ligaments, and tendons that work together to provide support and balance while walking, standing, or engaging in physical activities. Arch pain can occur in different parts of the foot, such as the medial arch (inner side of the foot), lateral arch (outer side of the foot), or metatarsal arch (ball of the foot).
Seeking effective treatment is crucial to regaining your mobility and quality of life. In this article, we delve into orthopaedic solutions and foot arch pain treatment designed to provide relief.. Whether you’re grappling with the effects of pes planus or seeking targeted solutions for your foot arch pain, we explore how orthotics and orthopaedic interventions can help alleviate your discomfort.

Source:https://www.freepik.com/free-photo/beautiful-women-feet-isolated-white-closeup_20987949.htm#query=foot%20arch%20pain&position=1&from_view=search&track=ais
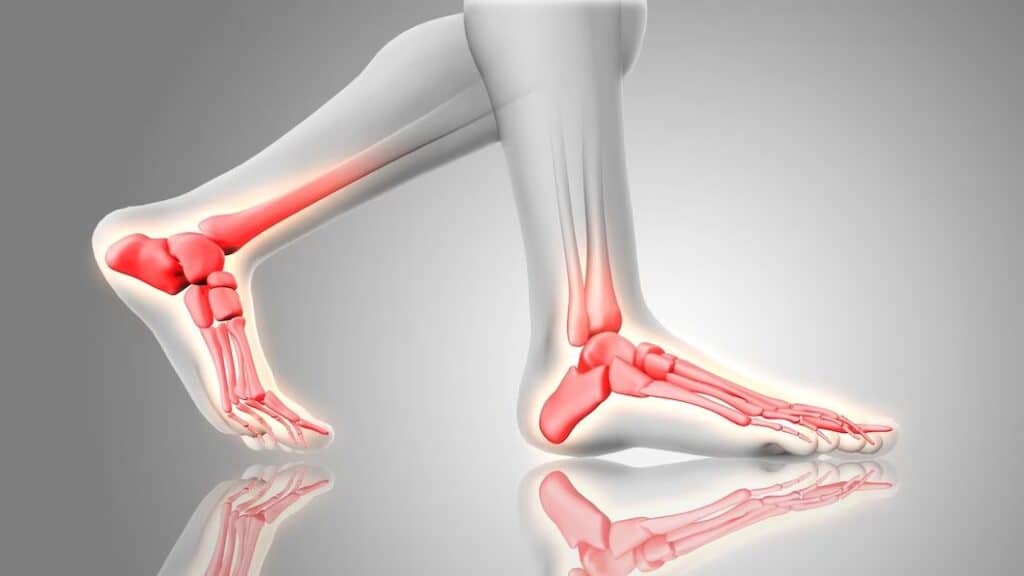
Arch pain is complicated with myriad causes in adults. One of the most common causes in Adults is adult acquired flatfoot or tibialis posterior tendon dysfunction. The tibialis posterior tendon is an important tendon on the inside of the foot and ankle which helps to support the medial (inner) arch of the foot. Weakness and dysfunction of the tibialis posterior tendon leads to pain and eventual collapse of the medial arch of the foot. PTTD is the most common cause of adult-acquired flatfoot.
Source:https://www.freepik.com/free-photo/3d-render-feet-close-up-with-glowing-bones_22918344.htm#query=foot%20arch%20pain&position=7&from_view=search&track=ais
Repeated strain can harm the posterior tibial tendon. As you age, the tendon can wear out. If you’re overweight, the extra weight can speed up the deterioration. And if you have had an ankle, foot or joint injury in the past, this can also make the tendon much more fragile. It’s not usually seen in younger people, and usually only occurs after an injury.
Adult pes planus is a condition where the arches of the feet flatten out, leading to an altered foot structure and potential discomfort. The arches of the feet play a pivotal role in maintaining the body’s balance, absorbing shock, and facilitating smooth movement. When these arches collapse or become less pronounced, it can result in strain on the muscles, ligaments, and tendons in the feet, leading to pain and discomfort. The development of adult acquired pes planus is usually multi-factorial. There can be a familial component, where genetic predisposition to the condition might be inherited.

Source:https://www.freepik.com/free-photo/3d-render-feet-close-up-with-glowing-bones_22918344.htm#query=foot%20arch%20pain&position=7&from_view=search&track=ais
Your doctor will check if there’s any swelling in your ankle and foot along the back of your lower leg. They’ll move your foot around and check out your ankle’s range of motion. Swelling, tenderness, pain, or weakness while you move your foot or ankle could be early signs of PTTD. They’ll check out your foot from behind to see if there’s any changes in shape or structure. Your heel might point outwards, and your inner arch may be flat on the ground. The front of your foot may move away from your body to balance out the changes to the heel and inner arch. From behind, your provider will also look for a “too many toes” sign. Normally, only the pinky toe and part or all of the ring toe are visible on the outside. But in people with PTTD, more toes might be showing.
The doctor will assess tightness of the calf muscles and of the achilles tendon, flexibility of the foot, strength of the tibialis posterior tendon, and heel alignment. To check the health of your posterior tibial tendon, you can do a single-limb heel rise test. Stand next to a wall or chair for balance, then lift your healthy foot off the ground and try to raise onto the toes of your affected foot. With a healthy tendon, you should be able to do 8-10 heel raises comfortably. But if you’re in the early stages of PTTD, you might not even be able to do one.
Your doctor can use imaging tests to figure out what’s going on with your feet, like X-rays to check for arthritis or fallen arches and MRIs to check out the tendon and muscles around it. An MRI can also be used to plan non-surgical or surgical treatments depending on the stage of the PTTD.

Source:https://www.freepik.com/free-photo/medical-massage-foot-physiotherapy-center_1319028.htm#query=foot%20arch%20pain&position=38&from_view=search&track=ais
Orthopaedic surgeons play a crucial role in treating various stages of foot arch pain, particularly in the case of disorders like adult acquired flatfoot or tibialis posterior tendon dysfunction. These medical professionals specialize in diagnosing and addressing musculoskeletal conditions, making them well-equipped to provide comprehensive care for individuals experiencing arch pain.
When it comes to foot arch pain, orthopaedic surgeons are skilled in evaluating the underlying causes through a combination of physical examinations, medical history assessments, and diagnostic imaging. They can accurately diagnose the condition and its severity, enabling them to tailor a treatment plan to the patient’s unique needs.
In the early stage where there is weakness of the tendon, medications, injections, shoe orthotics and physiotherapy can be prescribed to aid in recovery. Orthopaedic surgeons can design and provide custom orthotic devices, such as shoe inserts or arch supports. These devices help provide additional support to the arch, alleviate strain on the tibialis posterior tendon, and improve overall foot alignment.
When the disease becomes more advanced with collapse of the arch. Surgery to repair damaged tendons, realign and restore the arch maybe necessary depending on severity
Surgery may become necessary, if there is severe pain over the foot which does not respond to other non-surgical alternatives. It will depend on the stage of severity of the disease. This can range from simple tendon debridement procedures for early stage disease, to realignment procedures and tendon transfers for more advanced disease. In end stage disease, fusion of part of the joints in the foot may be necessary.
Here are some key factors to consider when contemplating surgery for severe foot arch pain:
Persistent Pain: If you’ve been experiencing persistent and severe foot arch pain despite undergoing conservative treatments such as rest, physical therapy, and orthotic devices, surgery may be an option to alleviate your discomfort.
Impaired Mobility: Severe foot arch pain can lead to limited mobility and difficulty performing everyday activities. If your pain is significantly impacting your ability to walk, stand, or engage in physical activities, surgery might be worth considering.
Worsening Deformity: Some conditions, like adult acquired flatfoot, can cause a visible change in the alignment of the foot and arches. If you notice a progressive deformity that is affecting your foot’s structure and function, surgery may be necessary to correct it.
It’s important to note that surgery is usually considered after a thorough evaluation by a qualified orthopaedic surgeon. The surgeon will assess your medical history, perform a physical examination, and may request imaging tests to determine the extent of the damage and the most appropriate surgical approach.
Orthotics, medications, injections and physiotherapy all have important roles to play in the management of adult acquired flatfoot. In the early stages of the disease, these might be the primary treatment modalities, which are focused on recovery of posterior tibialis tendon function In later stages of the disease, these modalities might still be necessary as supportive adjuncts to surgical treatment of the disorder.
If you’re experiencing pain and inflammation, you should try some over-the-counter non-steroidal anti-inflammatory drugs like aspirin, ibuprofen or naproxen. But check with your doctor first to see if it’s safe for you to take them. Doing some physical therapy exercises can also help you strengthen your tendon, and wearing shoe inserts or braces can give your tendon and arch extra support. Your doctor might even suggest you use a cast or walking boot, or a custom orthotic brace that fits your feet perfectly.
Physiotherapy is an important part of treatment for arch pain. Stretching of tight calf muscles and tendons help to reduce the amount of deforming force on the foot as it comes into contact with the ground. Stretching and strengthening of the tibialis posterior tendon and other supportive tendons help to restore function and relieve pain from acquired adult flatfoot. For those seeking non-invasive and holistic approaches to managing foot arch pain, physiotherapy presents an array of benefits that extend beyond mere symptom relief.
Comprehensive Assessment: Physiotherapists are skilled at conducting comprehensive assessments to identify the root causes of foot arch pain. They consider factors such as foot structure, gait, muscle imbalances, and biomechanics to develop a tailored treatment plan.
Customized Treatment Plans: Each individual’s foot arch pain is unique, and physiotherapists design personalized treatment plans to address specific concerns. These plans may include a combination of exercises, stretches, manual therapies, and education on proper footwear.
Pain Management: Physiotherapy focuses on alleviating pain by targeting the sources of discomfort. Through various techniques, physiotherapists work to reduce inflammation, ease muscle tension, and promote circulation, all of which contribute to pain relief.
Muscle Strengthening and Conditioning: Weak or imbalanced muscles can contribute to foot arch pain. Physiotherapists guide patients through exercises that strengthen the muscles supporting the foot arch, enhancing stability and reducing strain.
In conclusion, finding relief from foot arch pain is achievable through a combination of modern orthopedic techniques, pain management strategies, and appropriate lifestyle adjustments. Whether you opt for conservative treatments like orthotics, physiotherapy, or customized exercise routines, or if surgical intervention becomes necessary for severe cases, the ultimate goal is to regain pain-free mobility and enhance your quality of life. Consulting with a qualified orthopedic specialist is crucial to developing a tailored treatment plan that addresses the root cause of your foot arch pain and provides you with effective, lasting results. With the right approach and expert guidance, you can step into a future where foot arch pain is no longer a hindrance, allowing you to enjoy every step you take.
Foot arch pain is characterized by discomfort or soreness in the arch of the foot. The most common symptoms of foot arch pain include a sharp or stabbing pain near the heel or arch, especially after periods of rest or when taking the first steps in the morning, pain over the inside of the foot and tightening of calf muscles. The pain may radiate up to the inside of the ankle. It may gradually subside as you move around, only to return after extended periods of standing, walking, or physical activity.
Exercises can play a crucial role in managing foot arch pain symptoms and promoting overall foot health. Stretching of the calf muscles and the tibialis posterior tendon, which is a tendon running on the inside of the foot to the inner portion of the ankle are particularly beneficial for relieving tension in the plantar fascia—the band of tissue that runs along the bottom of the foot. Calf stretches, where you gently lean against a wall with one leg extended behind you, can help improve flexibility and reduce strain on the arch.
Surgery for foot arch pain is considered when more conservative treatment methods have proven ineffective in alleviating the pain and improving the patient’s quality of life. If symptoms persist or worsen despite efforts like rest, orthotics, physical therapy, and medication, surgical intervention might be recommended. Severe cases of foot arch pain that significantly impact daily activities, mobility, and overall well-being might also warrant surgical evaluation. Surgery can be an important treatment option at all stages of the disease. In general, surgery should be considered in earlier stages of the disease if non-surgical options fail. In later stages of the disease, surgery is usually the primary option for treatment.
The frequency of follow-up appointments with an orthopedic professional during recovery from severe foot arch pain can vary based on individual circumstances and the treatment offered. Surgical candidates will be followed up closely for the first 2 weeks after surgery for wound complications. Once the surgical wounds have healed, they will be referred for physical therapy, and will be followed up on a monthly to 2 monthly basis until symptoms have improved. This might involve visits every few weeks to assess healing progress, manage pain, and monitor any potential complications. Non-surgical patients undergoing physiotherapy will be followed up on a 2 to 3 weekly basis until symptoms have improved.
Diet and nutrition play a significant role in influencing the severity of symptoms related to foot arch pain. The foods we consume can impact inflammation levels, overall health, and the body’s ability to manage pain. Certain dietary choices can either alleviate or exacerbate foot arch pain. An anti-inflammatory diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce overall inflammation in the body, potentially alleviating pain and discomfort in the foot arch. On the other hand, a diet high in processed foods, sugary snacks, and unhealthy fats can promote inflammation, worsening pain. Maintaining a healthy weight for gender and size will help to minimize symptoms of adult acquired flatfoot. Adequate intake of nutrients like calcium and vitamin D is essential for maintaining strong bones, which can contribute to foot arch pain if deficient
Developing a personalized treatment plan is crucial for maximizing long-term recovery and relief from foot arch pain. First and foremost, consulting with a qualified orthopaedic professional is essential to accurately diagnose the underlying cause of the pain and tailor a comprehensive plan. A frank discussion with your surgeon with regards to your aims and expected outcomes will allow us to tailor a treatment plan best suited to you. Customized exercises can help strengthen the muscles supporting the arch and improve overall foot function. Physical therapy sessions under the guidance of a trained therapist can aid in addressing specific issues and tracking progress. Orthotic devices, such as arch supports or shoe inserts, can provide additional support and alleviate pressure on the arch.
For individuals with limited mobility, managing foot arch pain requires a tailored approach that takes their unique circumstances into account. First and foremost, seeking guidance from a medical professional or orthopaedic specialist is crucial to ensure an accurate diagnosis and appropriate treatment plan. Since limited mobility can restrict certain activities, it’s essential to focus on gentle exercises and stretches that can be performed comfortably.
Assistive devices and orthotics can play a crucial role in alleviating symptoms of foot arch pain. Custom-made orthotic insoles, arch supports, and shoe inserts are designed to provide proper support and alignment to the foot’s arch, distributing pressure evenly and reducing strain on the affected area. These devices help to stabilize the foot and improve its biomechanics, which can in turn ease discomfort and pain. Additionally, specialized footwear such as shoes with cushioning, shock absorption, and arch support can contribute to better arch alignment and reduce the impact on the arch during walking and other activities. In the early stage of the disease, arch supports, whether custom or off the shelf, can be considered to help support the arch and minimize foot pain with exercise or activities.

Dr Yong Ren graduated from the National University of Singapore’s Medical faculty and embarked on his orthopaedic career soon after. Upon completion of his training locally, he served briefly as an orthopaedic trauma surgeon in Khoo Teck Puat hospital before embarking on sub-specialty training in Switzerland at the famed Inselspital in Bern.
He underwent sub-specialty training in pelvic and spinal surgery, and upon his return to Singapore served as head of the orthopaedic trauma team till 2019. He continues to serve as Visiting Consultant to Khoo Teck Puat Hospital.
Well versed in a variety of orthopaedic surgeries, he also served as a member of the country council for the local branch of the Arbeitsgemeinschaft für Osteosynthesefragen (Trauma) in Singapore. He was also involved in the training of many of the young doctors in Singapore and was appointed as an Assistant Professor by the Yong Loo Lin School of Medicine. Prior to his entry into the private sector, he also served as core faculty for orthopaedic resident training by the National Healthcare Group.
Dr Yong Ren brings to the table his years of experience as a teacher and trainer in orthopaedic surgery. With his expertise in minimally invasive fracture surgery, pelvic reconstructive surgery, hip and knee surgery as well as spinal surgery, he is uniquely equipped with the tools and expertise necessary to help you on your road to recovery.