Diagnosing this form of bursitis is much like any other diagnosis of bursitis, but should be done with extra caution. If the affected elbow is punctured in order to remove any fluid, it is imperative that the area in which the procedure was done on does not become infected. Infected bursitis is much more serious than clean bursitis and can be very difficult to treat, and much more painful for the patient. Clean olecranon bursitis will yield a yellow-greenish fluid if removed, and tests on this fluid, be it from an x-ray or a lab test, should confirm if the affected elbow has olecranon bursitis or another form of bursitis. This will help ensure that whatever treatment the patient receives, it will have full effect on the bursitis.
Olecranon bursitis can occur in anyone across different age groups. For the most part, however, the issue affects grown adults and is most commonly associated with repeated pressure on the back of the elbow. This can lead to some uncomfortable sensations or even pain. Those dealing with the issue may also notice redness or warmth around the affected area, and it is even possible for there to be a fever present. One other sign of olecranon bursitis is the appearance of a lump on the affected elbow. This lump is due to the projection of the swollen bursa sac and can definitely be felt when pressed upon. If you are experiencing any of these symptoms, there is a good chance you may have olecranon bursitis.
Nerve pain in the elbow usually hinges on an irritation of the ulnar nerve that rests at the back of the elbow. This is known as Cubital Tunnel Syndrome. It may also be due to irritation of the radial nerve, most commonly at the front of the elbow. Nerves can be irritated by external pressure or some internal problem. External pressure is usually from prolonged leaning on the elbows, or repetitive bending of the elbow. An internal problem could be anything that takes up space in and around the elbow, e.g. swelling of the elbow joint following injury, or arthritis of the elbow. Frequently, patients are unable to recall a specific incident that may have caused the problem. Symptoms of nerve pain around the elbow will depend on which nerve is affected. If the radial nerve is affected, there may be pain at the front of the elbow, with some radiation down the forearm. The patient may experience numbness or tingling that affects the back of the hand or possibly the thumb and index finger. Ulnar nerve irritation typically causes pain at the back of the elbow, which may be quite acute. This may be associated with some numbness or pins and needles in the little and ring fingers.
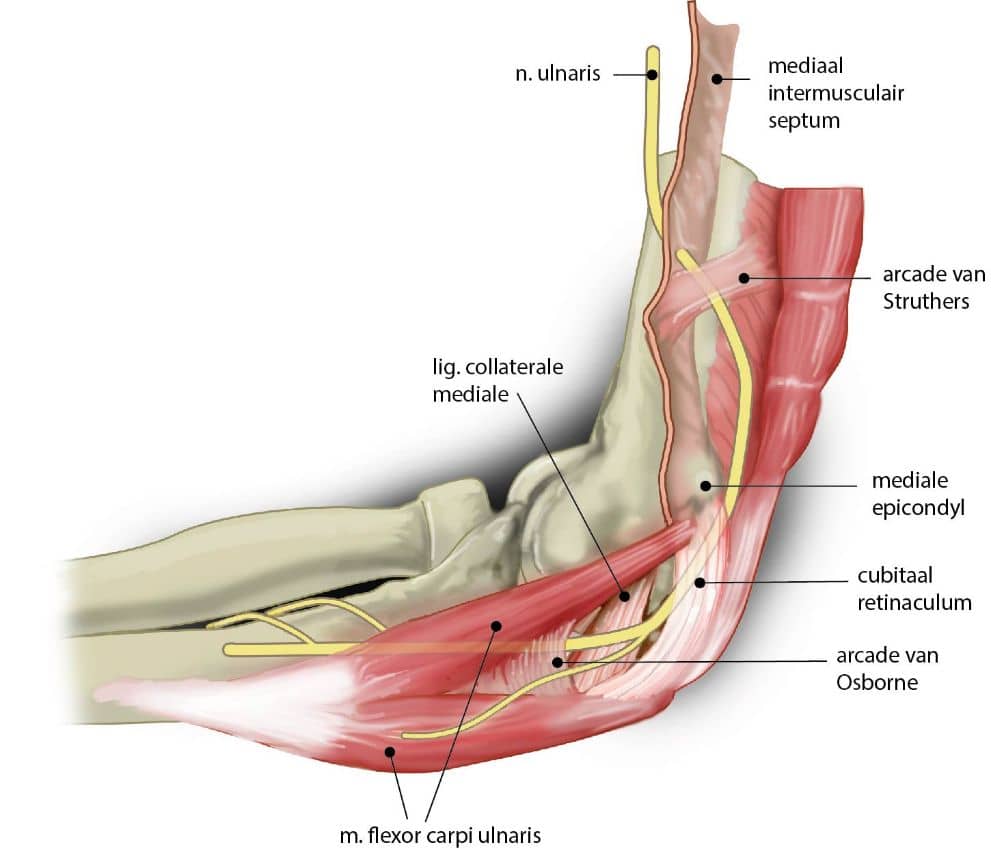
(image source: anatomytool.org)
The ulnar nerve is the most frequent site of compression in the arm. Different sites of nerve compression will cause different signs and symptoms. When the nerve is pinched in the cubital tunnel, it produces pins and needles in the little and ring fingers. This is often worse at night and may wake the patient from sleep. Severe compression can cause wasting of the small muscles of the hand, resulting in clawing of the ring and little fingers. If the compression is prolonged, a fixed claw deformity may develop and the strength in the grip may be lost. Compression higher up in the arm can cause symptoms in the upper arm and weakness of some of the muscles in the forearm. Common peroneal nerve compression typically occurs at the fibular head. The patient may be quite unaware of the cause of the foot drop. The cause can again be due to prolonged pressure. Individuals who are intoxicated or have insensibility are at increased risk of nerve palsies due to the fact they may remain in one position for a prolonged period and be unaware of discomfort due to pressure on a nerve. Nerve palsies can also occur as a complication of other diseases or illnesses. For example, a patient with an unconscious fit may sustain a brachial plexus injury. Individuals who present with what appear to be multiple nerve entrapments may need investigation for causes related to systemic illnesses. For example, diabetes and vasculitis are more known to cause multiple nerve entrapments.
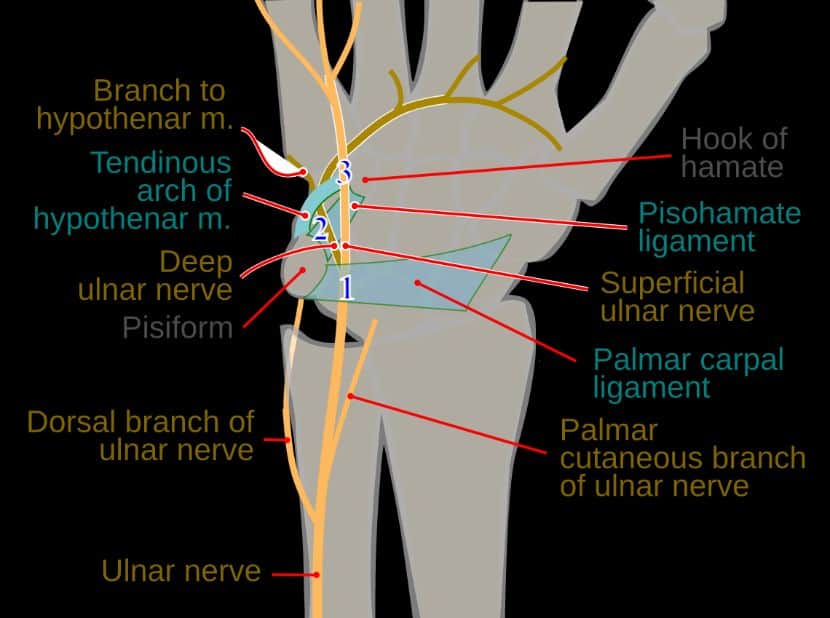
(image source: commons.wikimedia.org)
If a patient elects to proceed with surgical therapy, then the decision-making process for type of surgical procedure and the location of surgical treatment can be complex. The surgeon needs to determine if the lesions at the elbow are truly the primary source of symptoms and only then can it justify surgical release. Patients with primarily axonal lesions often have less predictable post-operative recovery and this needs to be communicated to them before getting consent for surgical therapy.
More controversial treatments are use of a formal elbow flexion pad and avoidance of prolonged or frequent elbow flexion. Recent advances include use of low-level laser therapy and therapeutic ultrasound. Corticosteroid injection is widely used and may be effective in some patients with mild symptoms. If the nerve conduction study shows worsening lesions, then such treatment should be discontinued and surgery discussed.
There are a variety of non-operative and operative methods to treat cubital tunnel syndrome. The primary goal of treatment in each case is to reduce the pressure on the ulnar nerve. Non-operative options include activity modification, use of a padded foam elbow splint, and a corticosteroid injection. If the lesion is mild or intermittent, then simply avoiding exacerbating factors or activities may suffice. A nightly elbow splint is done get to by some patients may help keep the elbow in.
The diagnosis of cubital tunnel syndrome involves taking a careful history and through clinical examination. An electrodiagnostic study is a very important adjunct to the clinical examination. It is common for patients to have ulnar neuropathy at the elbow as well as in different locations such as the wrist. The clinical examination may be suggestive of ulnar nerve symptoms at the wrist. An electrodiagnostic study should demonstrate that there is no ulnar neuropathy at the wrist. The study will also give information as to whether the neuropathy is primarily axonal. This is important because patients with predominantly demyelinating neuropathies respond better to surgical therapy than do those with primarily axonal neuropathies.
Pain relief and a decrease in muscle spasm can be achieved in 10-30 minutes, longer than this is unnecessary and could ultimately be damaging to the tissues, especially if the ice/compression is too tight. Too much ice application can reduce tissue extensibility to a point that could be counterproductive to the stretching techniques in the rehabilitation phases. 3-4 times a day for 15-20 minutes every time is a good guideline to follow for the first 48 hours. This should be continued until the pain alleviates and there is no morning stiffness. A crushed polystyrene foam cup of water that has been frozen then peel back the top of the cup to expose the ice can make an easy-to-hold handle and mess-free ice massage. Later in the rehabilitation, cold sprays and patches make an easy-to-use method of pain relief before and after exercise.
Application of ice or cold therapy to the elbow is a very old and still effective method of treatment for elbow pain, especially the type of pain that comes on suddenly (acute). Most people understand that ice is the best immediate treatment for a new injury, although many have been advised to use heat. There is rarely an occasion to use heat on elbow injuries. Ice decreases inflammation, muscle spasm, and pain. It does this by causing the blood vessels to constrict (frostbite is extreme vasoconstriction), reducing blood flow to the tissue. This limits the amount of inflammation that can occur. When the ice is subsequently removed, the blood vessels dilate (reactive vasodilation) bringing with it a clean sweep of the chemicals and debris produced by these inflammatory processes. Ice should be applied to the painful area in the form of crushed ice in a plastic bag or frozen peas, and will be more effective if combined with a compression bandage.
An elbow pad can work as an excellent protectant for the ulnar nerve. It can serve to cushion the nerve from outside pressure. Pressure on the ulnar nerve can cause symptoms in the ulnar aspect of the forearm, hand, and fingers. Ulnar nerve symptoms include pain, numbness, tingling, and weakness. Pressure on the ulnar nerve can also cause symptoms in the elbow itself, because the ulnar nerve provides sensation to the skin over the medial olecranon. This can cause symptoms when leaning on the elbows. Symptoms occurring when leaning on the elbows are often from the nerve becoming trapped between the skin and the bone, and can eventually be a cause of ulnar nerve compression. An elbow pad can also serve to keep the elbow warm, which can be beneficial to promoting blood flow and healing in an area of nerve compression. Warmth can also help to decrease nerve sensitivity.
Each of these exercises attempts to move the specific nerve through a full range of motion with the least possible irritation. High levels of pain during or after these exercises may not be well tolerated by the nerve. In such cases, it is best to see which motion caused the pain and try a different exercise that moves the same part of the nerve with less tension.
There are 7 basic nerve gliding exercises. These are: 1) Neck Extension – Nerve Glide. 2) Shoulder Depression – Nerve Glide. 3) Shoulder Abduction – Nerve Glide. 4) Shoulder Horizontal Abduction – Nerve Glide. 5) Elbow Extension – Nerve Glide. 6) Wrist and Finger Extension – Nerve Glide. 7) Resisted Forearm Supination – Nerve Glide.
A nerve easily becomes adhered and bound down along its path, restricting movement and causing local pain in the region of the body where the nerve is impinged. Such is the case with radial tunnel syndrome and posterior interosseous syndrome. Nerve gliding exercises are thought to help restore the nerve’s ability to glide smoothly through the surrounding tissue. This, in turn, should help the nerve move in and around the area of pain without becoming irritated. Before starting these exercises, it is a good idea to first identify which specific nerve is causing the symptoms. This may require assistance from a physical or occupational therapist. It is also a good idea to first attain pain relief, increase the range of motion of the elbow, and strengthen the muscles around the elbow before nerve gliding is started. This may ensure that the exercises are well tolerated and increase the likelihood that the nerve will glide without becoming irritated.
10% of people with tennis elbow are resistant to non-surgical treatments, and for severe chronic sufferers, surgery may become a consideration. With the vast majority of tennis elbow patients, a period of waiting to see if the condition subsides is recommended. This is a good approach, as half of all patients will improve within a year, and only 5% of patients who have waited will require surgery.
Injection Techniques Steroid injections should be considered in patients who have pain or stiffness that is irritating and affecting sleep or daily activities. They can be given or guided by the doctor through a variety of different ways, including the veins near the elbow joints, injecting straight into the upper forearm, or the most common method of injecting into the common extensor origin. This method involves treating the point where the extensor muscles originate from the lateral epicondyle and is voice of the elbow through the holes in the radial head.
Steroid injections for tennis elbow treatment are another, more invasive form of treatment. Basically, the injection is a higher dose of anti-inflammatory medicine and works by reducing swelling and decreasing pain. According to studies provided by the Cochrane Library, the effectiveness of steroid injections is uncertain. Although they show significantly better relief from pain and improved overall treatment in the short term compared to a placebo, no long-term effects are shown.
In the management of elbow pain syndromes, a variety of treatment methods have been employed, including various invasive approaches. Corticosteroid injection is the most widely used of these methods and there is evidence to suggest that it is effective in the short-term for conditions such as lateral epicondylalgia (LE) and ulnar neuropathy. Corticosteroids have a powerful anti-inflammatory action, theoretically reducing pain by reversing the pathological processes and improving function by reducing swelling and inflammation. By having a direct mechanical effect on the tissue, the volume of the injectate may be an important factor although there is a lack of evidence for this. Local anaesthetic is often mixed with the steroid to give short-term pain relief and help to diagnose the source of the pain. The duration and nature of the anaesthetic effect depends on the type of anaesthetic used, but in most cases it diminishes as the pain relief and anti-inflammatory effects begin to take place. The procedure of injections and injectates used are well tolerated in the conditions mentioned, with rare reports of adverse events. These include significant pain during the injection and increased pain for 24-48 hours post-injection; depigmentation and local fat pad atrophy with repeated injections and tendon rupture although the last of these is rare. Although high patient satisfaction rates have been shown post-injection and there is clear short-term benefit, questions about the long-term effects and efficacy mean that it is not a favored treatment option for ulnar neuropathy. Finally, it is stated that the treatment will not succeed in all cases and care must be taken to ensure that the failure of the injection is not misinterpreted as a treatment failure.
If conservative treatment of UCL elbow injury has failed, further surgical options can be considered, for example primary ligament repair or ligament reconstruction with tendon graft. Recent advances have now provided the option of UCL repair using Endobutton implant fixation. This procedure is minimally invasive and less traumatic than reconstruction, providing good outcomes and a high percentage success rate. Other studies indicate that the overhead throwing athlete responds well to UCL reconstruction with regard to return to pre-injury level and overall satisfaction. However, a variation in surgical technique depends on the method of tendon attachment and bone tunnel placement. High tension repairs placed isometrically with the flexor-pronator mass seem to produce the best clinical and subjective results.
Surgical treatment of UCL medial elbow nerve pain consists of rebuilding the normal anatomy of the elbow joint. The ulnar nerve may be surgically decompressed or transposed with a procedure called Cubital Tunnel Release. There are various techniques for this operation and involves taking tension of the nerve by lengthening the tunnel it passes through. The procedure may also require removal of any bony abnormalities compressing the nerve. Outcomes vary greatly with studies quoting between 70% and 90% good to excellent results.
Ergonomic adjustments involve altering the way daily tasks are performed with the intention of minimizing stress on the body. How does this relate to preventing elbow nerve pain? This can be explained with an analogy that’s commonly used by physicians. Johnson and Johnson describes elbows as a “simple hinge,” implying that it’s designed for a specific “range of motion.” This means that any stresses beyond bending and straightening the elbow can result in damage. For example, using the elbow to support the head in an awkward position while watching TV or sleeping can place a lot of pressure on the ulnar nerve. Over time, this can result in irritation of the nerve, as it’s not designed to withstand this type of stress, often leading to pain and numbness in the fingers. Another common scenario is leaning the elbows on a hard surface. The nerve is located very close to the skin just behind the elbow joint, and although it’s well protected in this region (this is why it’s commonly known as the “funny bone” since it’s actually a nerve sensation when the ulnar nerve is bumped), it is still susceptible to direct pressure with this sort of positioning. It’s clear that both these activities are beyond the “normal range of motion” for the elbow, and they’re easy to recognize as contributing factors to elbow nerve pain. Any activity that involves bending the elbow and putting weight on that bent elbow are risk factors for the development of compression-related elbow nerve syndromes.
Specific ergonomic adjustments are often tailored to an individual and their work environment. Some general recommendations for minimizing stress on the elbow include using the strongest (largest) joints/muscles available to perform a task, using tools that keep the wrist in a neutral position, and distributing weight evenly (using both hands) when lifting or carrying objects. A selection of general ergonomic tips for a range of tasks and tools are provided on this site. Each tip includes an image of the ergonomic adjustment and detailed information on how to implement it. The tips are divided into tasks that involve mainly repetitive movements, forceful exertions, prolonged static postures, and manual handling of loads. Click the links to try and identify ergonomic adjustments that may be beneficial for specific work tasks that aggravate your elbow pain.
Ergonomic adjustments involve modifying tools or performing tasks differently to alleviate joint or muscle strain. The primary goal is to keep joints in a ‘neutral’ position, so there is minimal stress on the surrounding tissues. If you are unsure whether certain tools or work tasks are contributing to your elbow pain, a health professional such as a physiotherapist or occupational therapist will be able to assess your work environment and make recommendations for ergonomic adjustments. In some cases, they may visit your work site to get a better understanding of your work tasks.
The first exercises are static stretching exercises. Static Stretching is a type of stretch that involves stretching a muscle to its point of discomfort and then holding the position. This is usually done by elongating the muscle and then applying slight pressure to increase the stretch. This can help increase range of motion of a joint and can be held for longer periods of time compared to other stretches. Static stretches are good at improving flexibility and can be used to aid in reducing muscle tension. This has the potential to increase a lot of pain to begin with and rapid progression may further increase current symptoms but in the long run these stretches can be very beneficial. Static stretching is recommended for golfers and throwers.
Stretching safely and effectively can lead to a decrease in pain and increase the strength in one’s elbow. Stretch is a form of physical exercise and any change in one’s physicality should be discussed with a physician. The ideas given in these stretching and strengthening exercises are general, and should not replace a specialist’s advice. These exercises should start off gradually and the amount of time doing them or weights used should be increased to challenge the muscles. Do not push or bounce a stretch as far as it will go and quick, jerky movements can damage the tissue. Stretches should be held for 10-30 seconds and should be performed at least 3-4 times. They can be held for as long as a few minutes and repeated up to 6 times. All movement should be slow and controlled.
The most common daily activities that involve prolonged elbow bending are working at a computer and talking on the phone. These damaged nerves will cause pain, numbness, tingling, and/or weakness in your elbow, forearm, hand, and/or wrist. When using a computer or any office equipment, always use the least force possible to press keys or move the mouse. The force of key strokes and mouse movements should be minimized. Padded covers can be installed on the mouse and the wrist rest on the keyboard to reduce pressure on the ulnar side of the wrist. The hands and elbows should be free from pressure. Ideally, the keyboard and mouse will be used on height-adjustable trays to position them as close as possible to elbow height so the hands and arms can be in line with the forearms. The shoulders should be relaxed and held down. Headsets or speaker phones should be used for the telephone to avoid cradling the handset between the ear and shoulder. When working at a computer whose position cannot be modified, it may be necessary to request a different job assignment. Task rotation or splitting a job with another employee may allow breaks from the positions that cause symptoms. Since reducing force, keeping the elbows free from pressure, and maintaining good posture are difficult to monitor while concentrating on computer work, it may be necessary to have someone observe and remind the patient. Cognitive functional therapy to retrain efficient movement strategies may be beneficial.
Preventative Measures
Given that much nerve-related elbow pain results from repetitive strain, injuries are typically more preventable than not. This means it is socioeconomically beneficial to strengthen and inform at-risk populations with simple lifestyle changes to avoid possible nerve pain development. Insight celebrating this clearly preventative focus can be obtained from professional lifestyles. Dentists unfortunately lose more hours due to musculoskeletal disorders than any other profession; over twice the probability of carpal tunnel syndrome occurrence can exist for dentists with five or more years of experience. To include as many risk factors as are currently available, a broad preventative list amounts to optimizing ergonomics of occupations, promoting more general lifestyle information, and ensuring a strong focus on elbow exercises to maintain overall joint health.
Regarding optimization, the elimination of elbow force and high grip repetitions decreases the probability of intra-limb nerve interaction. Certain professionals should therefore speak to an occupational therapist about daily behavior, with an aim to optimizing working conditions and making repetitions of the same strain less common. Office employees may wonder, similarly, what a break activity could be after using the computer or pen for extended periods of time. This would very likely be different for each person, which would ideally consist of a muscle activity opposite to the muscles used during working hours. Avoiding forward shoulder and internally rotated postures is also important to reduce nerve pressure. Stretching helps to lengthen muscles and thus counter muscle shortening. Keep company with health workers or any exercise professional to maintain proper technique, ensuring effective muscle lengthening only affects the stretched muscle. The Scapulohumeral Rhythm Protocol has been designed for office workers and can be reasonably seen as a first guide for reducing shortened muscle insufficiencies. This would be performed alongside some advised methods for taking regular breaks following a prolonged typing stint. Recommended general nerve stretching and general posture awareness for office workers is currently available for the neck, arms, wrists, and generally tips below the waist.
Ergonomic Adjustments
Ergonomic adjustments can help create a comfort-adapted living or work space. Ergonomics modifies the work site or activities to avoid strain on joints, muscles, nerves, and other soft tissues. It can prevent and lessen elbow, shoulder, wrist, and hand nerve pain problems. Proper workstation setups, keyboard use, tools, implements, and equipment use, good posture, work breaks, and regular exercise all play a part in reducing and preventing elbow nerve pain. Workstation setups adjust chair height, desk elevation, and monitor placement. Alternating between sitting and standing to work and talk to clients emphasizes the strength of multi-position sit-stand-lift desks, chairs, and bimodal seaters, gear, and accessories. Adjusting equipment duration, use, location, and technique can also reduce hand, wrist, and elbow nerve compression or irritation. Using the optimal lever, instrument, piece of equipment, low friction torque, carries, washes, or fabrics can decrease the amount of pressure it takes to complete a work or activity function. A rapid or single event injury, which can be treated with rest, ice, and a healthy diet, is much less likely to occur when your work habits are adapted to your work duties and personal preferences. Allow for periodic activity reviews to capture a proper ergonomic picture for safety, productivity, and long-term comfort. Individual ergonomic assessments focus on modifying the workspace to better fit an employee’s work style, job tasks, workstation furniture, and equipment. Ergonomists and qualified experts help people prevent or lessen job task repetition and force, poor posture, contact pressure, movement, task speed, genetics, and poor conditioning. Adjustments may be made to accommodate an employee’s job functions and postural and comfort preferences, reduce the risk of injury or muscle and tendon pain, perform more work tasks with less discomfort, or, in certain instances, provide reasonable accommodation for employee requests. Ergonomic studies can be especially useful for individuals who already suffer from an elbow, shoulder, or hand nerve problem. Suffering from one kind of nerve or blood vessel irritation increases the chance of developing a new injury or pain disorder. Retrofitting in and around an injured or problematic area is a good first step in preventing nerve and/or tissue problems from extending to other significant body locations. Tips for when ergonomic reviews are not available or are limited: Employees should adjust office and home chairs, keyboards, and desks to best fit their body size and joint and posture comfort. Always change postures, desks, and chairs frequently. Stand for a portion of the day rather than sitting for long periods. Place the keyboard directly in front of them with the mouse beside the keyboard rather than on the pulling edge. Sit comfortably with back support. Ensure your knees and hips are at about a 90-degree angle. Keep the monitor at arm’s length, centered, and at or slightly below eye level. Forceful exertions such as lifting weights should be kept to a minimum.
Lifestyle Changes
Maintaining healthy joints can go a long way in preventing many different kinds of joint pain. Another step that one can take is simply to listen to the type of pain you are feeling, as pain can evolve or be the result of certain activities. If you experience pain in your elbow and arm, consider stretching your muscles and changing your behavior to give your muscles a rest. Below are several things that can be helpful in preventing nerve pain that begins in the elbow and travels up the arm as part of comprehensive prevention and not necessarily directly applicable to the nerves that pass through the elbow. They are:
1. Balanced Lifestyle: Proper nutrition and weight management can help to reduce strain on your elbow. Your weight, occupation, and activities will play a big part in your personal course of treatment, so don’t forget to mention them to your doctor. Taking care of the rest of your body, including strengthening and stretching exercises, may also help to reduce elbow nerve strain. 2. Flexibility: Being more flexible can also take some of the load off your elbow and help the other muscles support the movement of your arm. Stretching is helpful here.
3. Periodic Rest: For those who need to use their hands in awkward positions or grip an object in bright sunlight, taking periodic rest breaks for the wrist and elbow may offer the nervous system periodic rest and help to lessen cumulative stress on that nerve.
Education is your best resource. When you can spare the time, check out seven things about your joints that are dots you need to be connecting to help you start to understand where problems come from and what can help you prevent them. These are the risk factors for repetitive stress, trauma, and inflammation that can contribute to nerve pain that starts in your elbow.
Exercises
Therapeutic exercises to improve the flexibility, strength, and endurance of the elbow muscles and prevent associated nerve pain:
1. Flexibility exercises
– Triceps stretch
Stand or sit up tall and place one hand at the back of your head. Apply gentle pressure to your elbow to increase the stretch in your triceps muscle.
– Wrist flexor stretch
Extend your affected arm in front of you at shoulder height, elbow straight, and palm facing upwards. Turn the hand to face downwards by gently pressing the back of the hand.
2. Strengthening exercises
– Bicep curls
Hold a light weight in your hand and stand or sit with good posture. Rest your arms down by your side and rotate them to hold the weight with your palm facing upward. Now slowly lift your palm to your shoulder and then lower it down.
3. Endurance
After exercising, perform stretches for the affected area to improve blood flow, increase the range of motion, and reduce stiffness. Regular workouts are advised to ensure correct posture and to learn the proper techniques. Start slowly and build up gradually to avoid exacerbating an existing issue. If done consistently, the techniques will be more effective at preventing the development of neck, shoulder, and elbow nerve pain.
· Signs and symptoms include numbness, tingling, and curved little and ring fingers.
· Patients may also experience medial sided elbow pain radiating to forearm, numbness especially over the little and ring fingers and numbness over the ulna border of wrist.
· These signs and symptoms may differ from person to person.
· See “Signs and Symptoms of Elbow Nerve Pain“ section above for more information.
· You can go for a consultation with an orthopaedic surgeon, protect your joints through padding the elbow, and identifying old elbow injuries.
· Additionally, you can perform warm up or stretching before activities and take breaks to manage your routine and lifestyle.
· Simple lifestyle changes can include avoiding resting the elbow on hard surfaces.
· See “Prevention Strategies to Reduce the Risk of Developing Elbow Nerve Injury” for a comprehensive guide.
· Yes, you can try avoiding extrinsic pressure to the elbow especially over the point of the elbow.
· Your orthopaedic surgeon may also recommend adjustments to your posture while using the injured arm.
· See “Lifestyle Changes to Manage Elbow Pain” for a complete explanation.
· Generic pain medications include non-steroidal anti-inflammatory drugs (like ibuprofen and aspirin) and opioids.
· Your orthopaedic surgeon may prescribe nerve modulators (such as pregabalin and gabapentin) and nerve supplements (including B-complex, Vitamin E and Alpha lipoic acid).
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for a complete list of medications.
· Yes, massage therapy helps in alleviating pain and discomfort.
· Massage therapy may be only one part of the treatment plan recommended by your orthopaedic surgeon.
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for a comprehensive list of potential treatments.
· One surgical technique is the anterior transposition of ulna nerve. The objective of this surgery is to alleviate symptoms and discomfort.
· In this surgery, an incision will be done on the elbow. Afterward, the ulnar nerve will be moved to a new position.
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for a comprehensive list of potential treatments.
· Yes, your age will affect the type and frequency of treatments.
· As you get older, your body changes. These changes affect the effectiveness of medicine and treatments.
· See “Risk Factors That Contribute to Elbow Nerve Pain” for more information.
· Acupuncture is effective for muscle related pain but does not have significant impact on nerve related pain.
· The acupuncture method uses thin needles are inserted into the skin at different locations and depths.
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for a comprehensive list of potential treatments.
· Bracing involves an orthopaedic device to immobilise a specific joint or body part to facilitate quicker healing.
· In some cases, there might not be an effective brace available for this condition. It is best to consult with your orthopaedic surgeon for effective advice.
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for additional details on treatments.
· For elbow nerve entrapment, the recovery of the surgical wounds takes 2 weeks.
· The timeline of nerve recovery will depend on the severity of the nerve injury.
· You may also have to attend regular check-ups with your orthopaedic surgeon to track your progress after surgery.
· Yes, you should seek medical care for this condition.
· Depending on your condition, you may need interventional treatments and/or non-interventional treatments.
· It is best to avoid self-medicating to prevent further complications.
· Most of the medications effective in this case are prescription only.
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for additional details on treatments.
· If there is severe damage to the nerve with chronic numbness or weakness of hand muscles, additional surgery including tendon transfers may be necessary.
· This may also be the solution for muscle loss, which is a severe condition.
· See “Surgical and Non-Surgical Treatments for Elbow Nerve Pain” for a list of potential surgical methods.
· The Orthopaedic & Pain Practice is here to address your musculoskeletal needs through personalised treatment plans and a multi-faceted approach to pain management. Reach out to us by contacting +65 9898 3595 for a consultation with an orthopaedic surgeon.

Dr Yong Ren graduated from the National University of Singapore’s Medical faculty and embarked on his orthopaedic career soon after. Upon completion of his training locally, he served briefly as an orthopaedic trauma surgeon in Khoo Teck Puat hospital before embarking on sub-specialty training in Switzerland at the famed Inselspital in Bern.
He underwent sub-specialty training in pelvic and spinal surgery, and upon his return to Singapore served as head of the orthopaedic trauma team till 2019. He continues to serve as Visiting Consultant to Khoo Teck Puat Hospital.
Well versed in a variety of orthopaedic surgeries, he also served as a member of the country council for the local branch of the Arbeitsgemeinschaft für Osteosynthesefragen (Trauma) in Singapore. He was also involved in the training of many of the young doctors in Singapore and was appointed as an Assistant Professor by the Yong Loo Lin School of Medicine. Prior to his entry into the private sector, he also served as core faculty for orthopaedic resident training by the National Healthcare Group.
Dr Yong Ren brings to the table his years of experience as a teacher and trainer in orthopaedic surgery. With his expertise in minimally invasive fracture surgery, pelvic reconstructive surgery, hip and knee surgery as well as spinal surgery, he is uniquely equipped with the tools and expertise necessary to help you on your road to recovery.
References
Dwyer, T. (2009). The Bone School. Retrieved from http://www.boneschool.com/
Hecht, M. (2018). Ulnar Nerve Entrapment. Retrieved from
https://www.healthline.com/health/lunar-nerve-entrapment#nonsurgical-treatment
Johns Hopkins Medicine. (2021). Cubital Tunnel Syndrome. Retrieved from
https://www.hopkinsmedicine.org/health/conditions-and-diseases/cubital-tunnel-syndrome
Lloyd, W. (2020). Orthopedic Rehabilitation. Retrieved from
https://www.healthgrades.com/right-care/bones-joints-and-muscles/orthopedic-rehabilitation
OrthoInfo. (2020). Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome). Retrieved
from https://orthoinfo.aaos.org/en/diseases–conditions/ulnar-nerve-entrapment-at-the-elbow-cubital-tunnel-syndrome/